Irregular bleeding is common during perimenopause. At first, cycles can be shorter by just a few days (25 vs 28 days, for example) or you may get your period every 3 weeks.
Most women will experience period changes as they move into perimenopause. Changes can range from irregular cycles, abnormally heavy or prolonged bleeding (menorrhagia), and / or increasingly painful cramps (dysmenorrhea) — and yes, this can happen even if your cycle ran like clockwork before. The culprit? Hormonal changes.

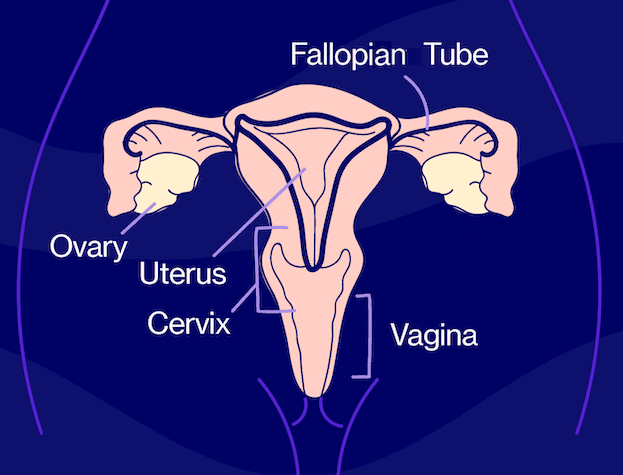
How your hormones play a role
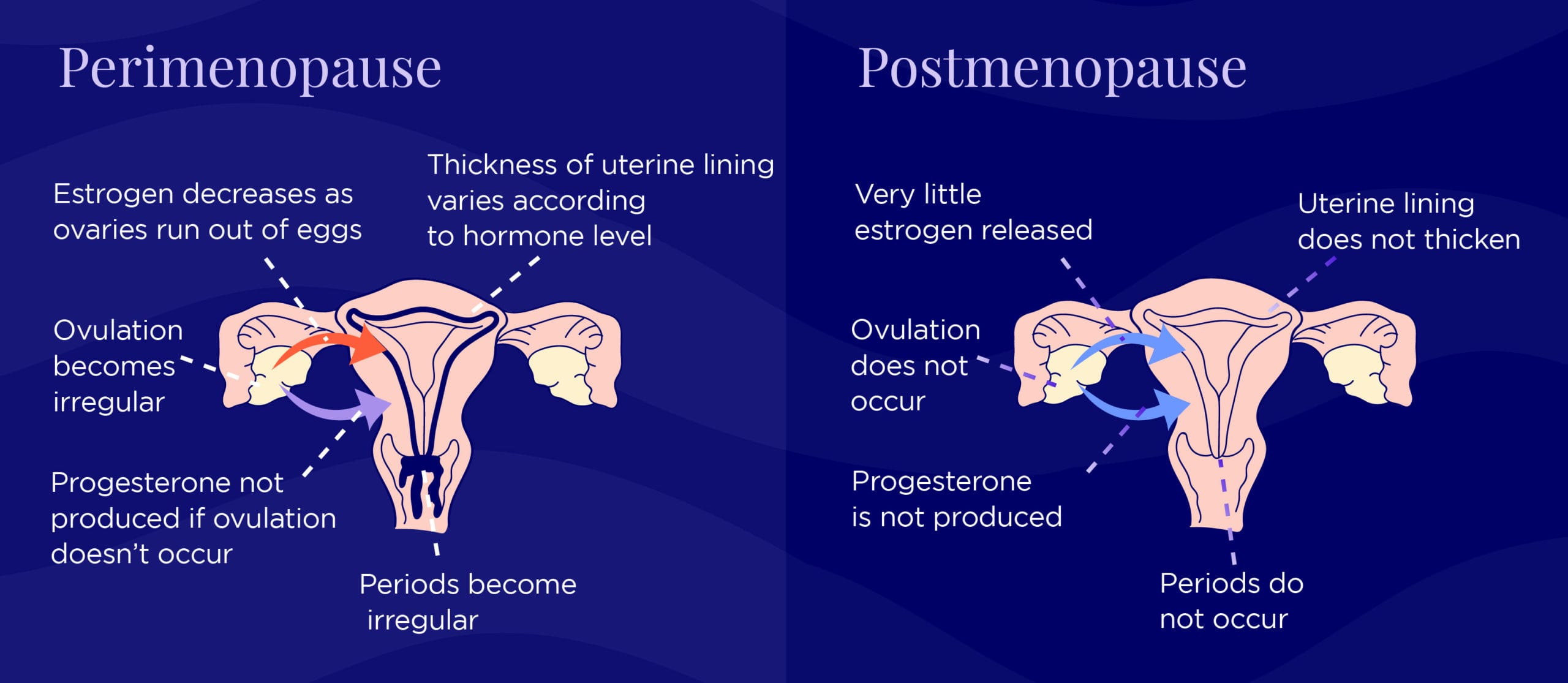
The two primary reproductive hormones for women, estrogen and progesterone, control menstruation along with a slew of other functions in our body. Among other things, estrogen causes the endometrial lining, or the lining of the uterus, to thicken during a typical menstrual cycle. Progesterone balances estrogen by controlling the build-up of the endometrium and preparing the lining for the potential of pregnancy. When hormone levels shift and eventually decline during the menopausal transition, the result is irregular periods. Below is an example of how some women experience the transition, but remember: everyone is different and your experience may be different.
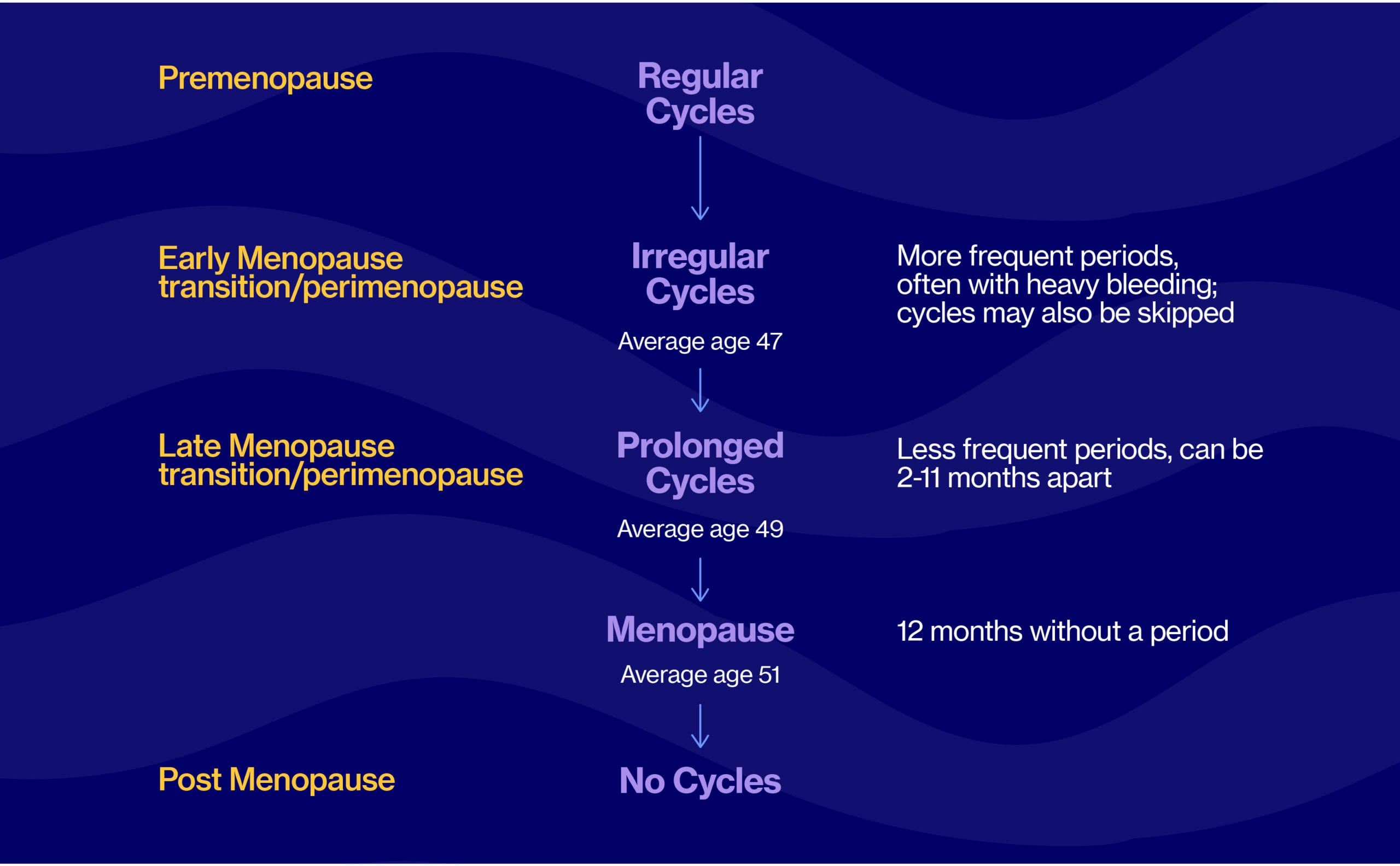
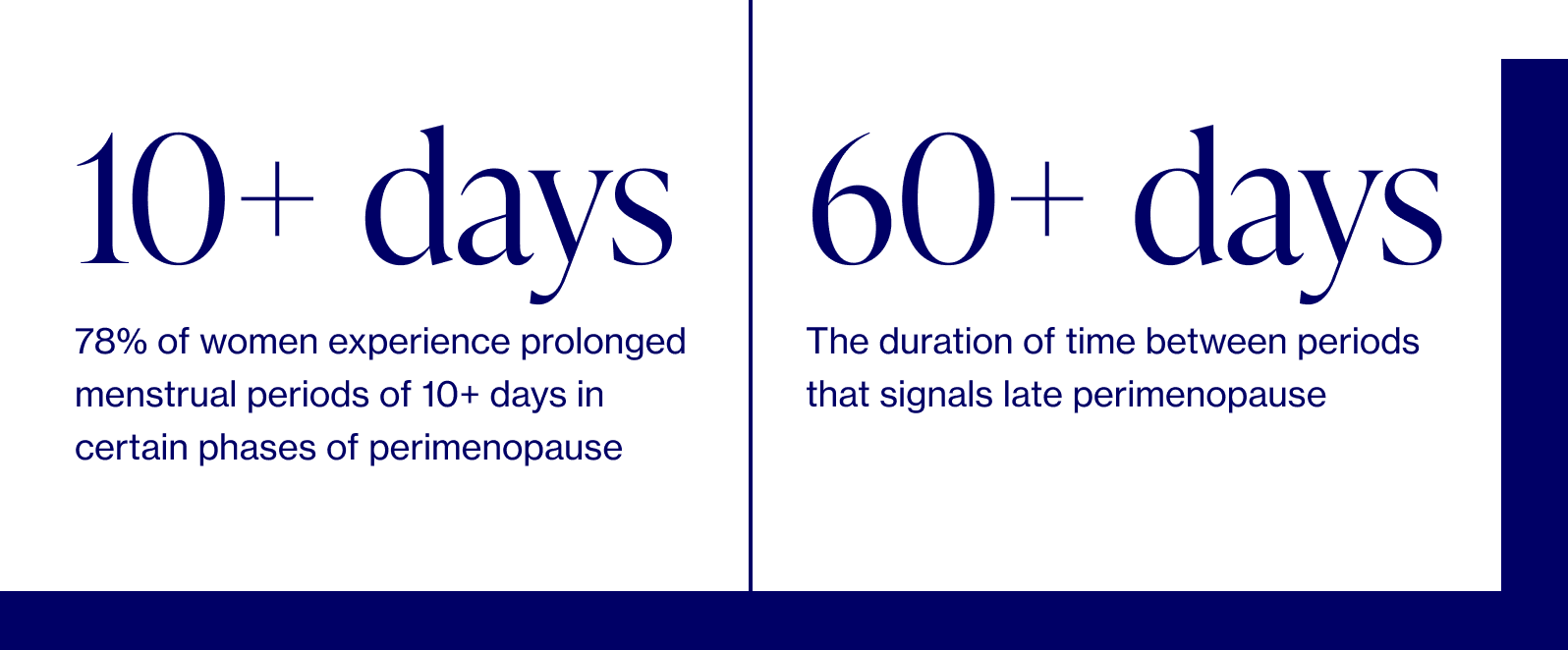
Typically, as early perimenopause shifts into late perimenopause and the last menstruation approaches, cycles become more irregular, and scarce due to declining estrogen levels, often absent ovulation, and less growth of the uterine lining. We unfortunately cannot test accurately for when that last period will come, but the average age tends to be around 51, marking the end of reproductive years. Some women will continue to menstruate well into their 50s.
How heavy is talk-to-your-doctor heavy?
Our bodies and our cycles vary tremendously, but here are some benchmarks to consider, especially if this type of bleeding is new and different from your baseline:
- Soaking through 1 pad/tampon per hour for 2+ hours
- Bleeding for longer than 1 week
- Passing blood clots larger than a quarter
- Waking up at night to change a pad or tampon
Below are two other reasons you may want to seek additional medical help:
- Prolonged, heavy, or painful periods can sometimes be a result of polycystic ovarian syndrome (PCOS), polyps, fibroids, coagulation (blood clotting) problems — in which case you should definitely consult your doctor.
- Any and all vaginal bleeding post-menopause is considered abnormal and should be a sign to talk to your doctor. While the cause could very well be harmless (like vaginal dryness), it could also be a signal of a more serious medical condition, including uterine cancer. If you have postmenopausal bleeding, you need to call your doctor right away. And if you can, bring notes on the length, duration, and flow of your bleeding to that doctor’s appointment.
Oh, and one more note on irregular periods
They could very well be due to other causes outside of perimenopause and menopause, including anything that can disrupt ovulation: thyroid and prolactin abnormalities, polycystic ovary syndrome (PCOS), adrenal problems, extreme stress, illness, etc.
Periods that suddenly become irregular may require a workup to exclude causes other than perimenopause, especially for women in their early 40s. And remember, while a skipped period at 40 may mean perimenopause (or any of the culprits listed above), it can also mean pregnancy!
Dr. Anna Barbieri, MD
Pro tip #1
Before your next annual visit, track your cycle for 1-2 months to share with your doctor. Tracking specific cycle length between periods, duration of your period, and flow can help your doctor better understand where you are in the perimenopause transition, or whether there is potentially something else that should be evaulated. For example, decreased time between cycles (< 28 days) could be an early sign of perimenopause, while increased time between periods often signals late perimenopause.