Published on Mar 19, 2021
Last modified on Mar 20, 2021
Pelvic health through the menopause transition and beyond
5 min read

Amy Stein, DPT, BCB-PMD, IF, author of the award-winning books, Heal Pelvic Pain and Beating Endo: How to Reclaim Your Life from Endometriosis, is a leading expert in pelvic floor dysfunction, pelvic pain, and functional manual therapy for people of all ages and genders.
She is the founder and owner of Beyond Basics Physical Therapy in New York.
Recently, Amy spoke with Elektra provider Jacqueline Giannelli, FNP about pelvic health during the menopause and beyond on Instagram Live. Amy wrote this blog post about urinary incontinence for the Elektra community.
View this post on Instagram
Urinary incontinence is common, but it’s not something you have to learn to live with!
We are going to cover three types of incontinence: stress incontinence, urge incontinence, and mixed incontinence. Treating your incontinence will improve your quality of life.

Stress incontinence
Stress incontinence is defined as urinary leaking with increased intra-abdominal pressure, from events such as coughing, sneezing, laughing, or physical exertion. This happens due to a weakness and/or shortening of our pelvic floor muscles. Pelvic floor muscles are the muscles that connect from the pubic bone to the tailbone which support the abdominal organs and assist in bowel, bladder, and sexual functionality. If you’ve given birth vaginally, your pelvic floor muscles may lengthen and weaken. This can result in urinary or bowel leakage.
Urge incontinence
Urge incontinence is the sudden, strong, and uncontrollable urge to urinate. Also known as “key-in-lock” syndrome, some people say they experience this as soon as they put their key in the door. This could be the result of shortened and weak pelvic floor muscles or from an increase in your normal muscle tone.
Mixed incontinence
Mixed incontinence refers to the combination of stress and urge incontinence.
So, can these problems be fixed?
YES! However, medication or surgery are not always the answer and sometimes can worsen symptoms. If you suffer from stress incontinence or decreased sexual stimulation, you need to strengthen your pelvic floor muscles, after being evaluated by a pelvic floor physical therapist (PFPT).
How to strengthen the pelvic floor
It’s all about exercise. Specifically, it’s about Kegels, named after Dr. Arnold Kegel, a gynecologist in the 1950s. There are two different types of muscle fibers in the pelvic floor. Therefore, you need to do two different types of Kegels:
- Endurance holds: holding for 10 seconds
- Quick holds: holding for 2 seconds
Repeat each exercise 10 times, 3-4 times per day.
Biofeedback, directed by a trained healthcare provider (physical therapist, nurse practitioner), can assist in understanding where these muscles are and how to do the exercises properly. They can also help you develop an exercise program specific to your needs. Physical therapists also address the entire musculoskeletal system, taking into account hip strength, core stability, and pelvic alignment. With specific exercises, your leakages should stop and your orgasms should improve.
Keep in mind that everyone responds differently. One person may achieve their goals within 2 months, and for another person, it may take 6 months.
Addressing urge incontinence
Urge incontinence usually requires a more hands-on approach by a physical therapist trained in the treatment of pelvic floor dysfunction. It’s usually a two-step process aimed to lengthen and strengthen your muscles. Urge incontinence is typically the result of shortened pelvic floor muscles, so first, these muscles need to be lengthened through myofascial trigger point release and connective tissue mobilization.
Then, you move on to the second step: strengthening them with Kegels and core stabilization exercises. If one strengthens the pelvic floor muscles prior to lengthening them, then their muscles will remain in the shortened position and their problem will persist.
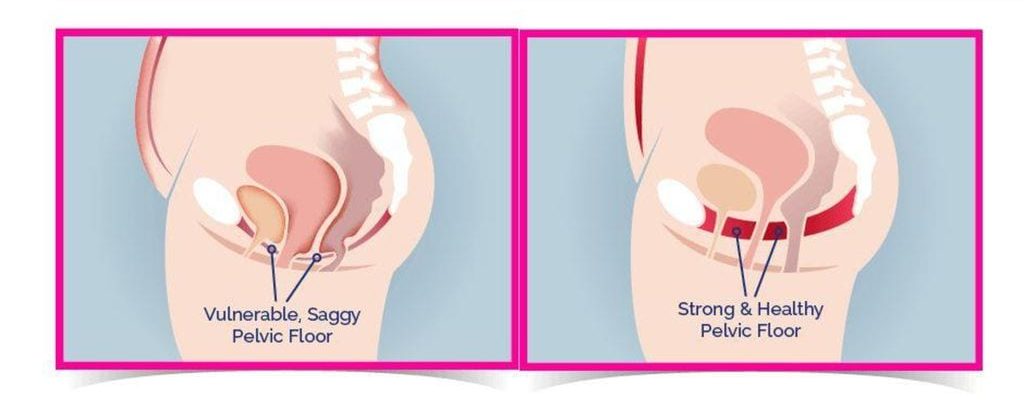
Prolapse (a descent) of the bladder, colon, or uterus may or may not contribute to the leakage. A prolapse is typically caused by weak or lengthened muscles and fascial tissue. This can also be helped through strengthening of the pelvic floor muscles (kegels).
A warning: Kegels are not the end all be all!
It’s completely intuitive that people would think Kegels would help incontinence. But incontinence does not necessarily mean you have weak pelvic floor muscles! Doing pelvic floor strengthening exercises without being evaluated by a PT can actually worsen your symptoms. Weak and loose pelvic floor muscles can be responsible for incontinence, but weak and tight muscles are as well.
When things get too tight
Tight pelvic floors have a decreased range of motion, which is necessary to generate the force you need to counteract the pressure from activities like lifting, coughing, laughing, and sneezing.
If you have pain in your pelvis that’s unrelated to a medical condition (keep in mind that tight pelvic floors can be related to many conditions), your pelvic floor is probably tight. A tight pelvic floor may also have trigger points which can send pain to various locations in your genitals, back, legs, and abdomen. Continuing to tighten can cause this pain to get worse. Instead of Kegels, try relaxation exercises and techniques such as pelvic floor drops.
How to do pelvic floor drops
A pelvic floor drops is the relaxation of the muscles of the pelvic floor. It is like that feeling you have when you can finally relax the muscle in between your legs after holding urine in for a long time. It’s a great feeling of relaxation and here’s how you can mimic it when you don’t have to go:
- Get comfortable. Sit, stand, lay down, or whatever suits you. Relax your body and close your eyes.
- Breathe deeply. Inhale for 3-5 seconds.
- Exhale slowly for 5-6 seconds. As you exhale, imagine that your breath is gently placing pressure on your pelvic floor in a relaxing manner. Don’t push or strain.
But wait, there’s more!
Here are a few additional tips for you to reduce incontinence and additional bladder dysfunctions.
Drink more water
It may sound counterintuitive, but drinking plenty of water is good for almost all bladder conditions. Yes, I am talking about leaking, urgency, incomplete emptying, and frequency. Hydrating keeps your urine nice and dilute, which minimizes the irritation of your bladder wall as well as the reactive spasm of the detrusor muscle.
Each day, you should drink approximately half of your bodyweight in ounces of water.
For example, a 150 lbs person should consume 75 ounces of water a day. If you are exercising, sweating, or drinking lots of caffeine or alcohol, you should increase this amount.
Avoid irritants
It is also important to be mindful of bladder irritants which can worsen bladder issues. Big irritant culprits are alcohol, caffeine, citrus, and spicy food.
Train your bladder
If you have bladder frequency or leakage, now is the time to try and train your bladder to hold more urine. Keep in mind, you should start treatment to address pain with physical therapy and in certain cases, with medication, to allow you to be successful with bladder training. I always tell my patients to start their bladder retraining at home, where a bathroom is available to take the stress out of possible leaks or not being able to find a bathroom.
Start by simply waiting to go to the bathroom 5-10 minutes past your first urge to urinate. Use behavioral strategies such as deep breathing, pelvic floor drops, mindfulness, and distraction and others.
If you don’t have to go after 5-10 minutes, great! If you do, go to the bathroom.
Once waiting 10 minutes becomes easy, extend your waiting time by 20 minutes until you are able to last 2-3 hours between urinating.
Exercise!
Exercise, especially strength training, is important! After age 60, we start losing muscle mass at a rate of approximately 15% per year. The less active someone is in their life, the quicker this loss occurs. But there is hope. Aging isn’t a slippery slope into weakness and frailty. It is what you make of it. Weight training can actually reduce fat and build muscle, helping to reverse the condition of sarcopenic obesity. Many studies even indicate that resistance training can prevent and or reverse age-related losses in function.
More than 50% of perimenopausal and menopausal people show signs and symptoms of genitourinary syndrome of menopause (GSM). These symptoms, caused by fluctuating estrogen levels, include vulvovaginal dryness, burning, irritation, decreased lubrication, painful sex, urinary urgency, recurrent UTIs, and painful urination.
In addition to receiving pharmacological treatment and using vaginal moisturizers and lubricants, GSM sufferers greatly benefit from a pelvic floor therapist who can prescribe exercises for bone and heart health and improve pelvic floor coordination.
A pelvic floor therapist will also address any muscle dysfunction caused or exacerbated by painful sex and assist in vaginal dilator therapy, which promotes the stretching of vaginal tissues. They’ll also go over sexual ergonomics like positioning and proper lubrication usage to help ease pain during intercourse.
Curious for more? Read Elektra’s guides to vaginal and urinary symptoms of menopause.
Resources
Chen M, Jiang B. Resistance training exercise program for intervention to enhance gait function in elderly chronically ill patients: multivariate multiscale entropy for center of pressure signal analysis. Comput Math Methods Med. 2014
Giangregorio G. Papaioannou A. MacIntyre N. Too fit to fracture: exercise recomendations for individuals with osteoporosis or osteoporotic vertebral fracture
Liao C, Tsauo J, Lin L, et al. Effects of elastic resistance exercise on body composition on body composition and physical capacitiy in older women with sacropenic obesity. Medicine. 2013. 96(23)
Mayer F, Scharhag-Rosenberger F, Carlsohn A. The intensity and effects of strength training in the elderly. Dtsch Arztebl Int 2011; 108(21):359-64


