Published on Apr 22, 2024
Last modified on Dec 22, 2025
Understanding the Connection Between Gut Health and Menopause
7 min read
Okay, we know everyone and their mother is talking about gut health. Probiotic ads are clogging our feeds, Instagram influencers are hawking products while decrying a gut health epidemic, and all the information can feel super overwhelming. Plus, most of it doesn’t touch on the complexities of gut health during menopause in particular. (Spoiler alert, our gut microbiome changes during the menopause transition).
Don’t worry, we’re not here to yell at you about healing your gut, buying unpasteurized milk, or starting a cleanse. But we do want to untangle some of the information out there around gut health and get to the bottom of what it means for us during menopause…
What is “gut health” and why is it all the rage?
Believe it or not, the term “gut health” is rarely used in scientific literature, but it IS used often within human medicine (aka real-life, non-clinical conversations). When we talk about “gut health,” we’re really referring to the overall health of the digestive system, specifically the small and large intestine. Within the large intestine, each of us has a unique microbiome composition.
Micro-what? Time for a quick bio crash course: A microbiome is essentially the collection of genomes of microorganisms within a given environment–in this case, the gut.
So, our gut microbiome compositions vary and generally, having a diverse collection of gut bacteria microbes is associated with good digestive health. Some studies have also suggested a relationship between reduced gut microbiome diversity and Irritable Bowel Syndrome (IBS).
 Source: Harvard Health
Source: Harvard Health
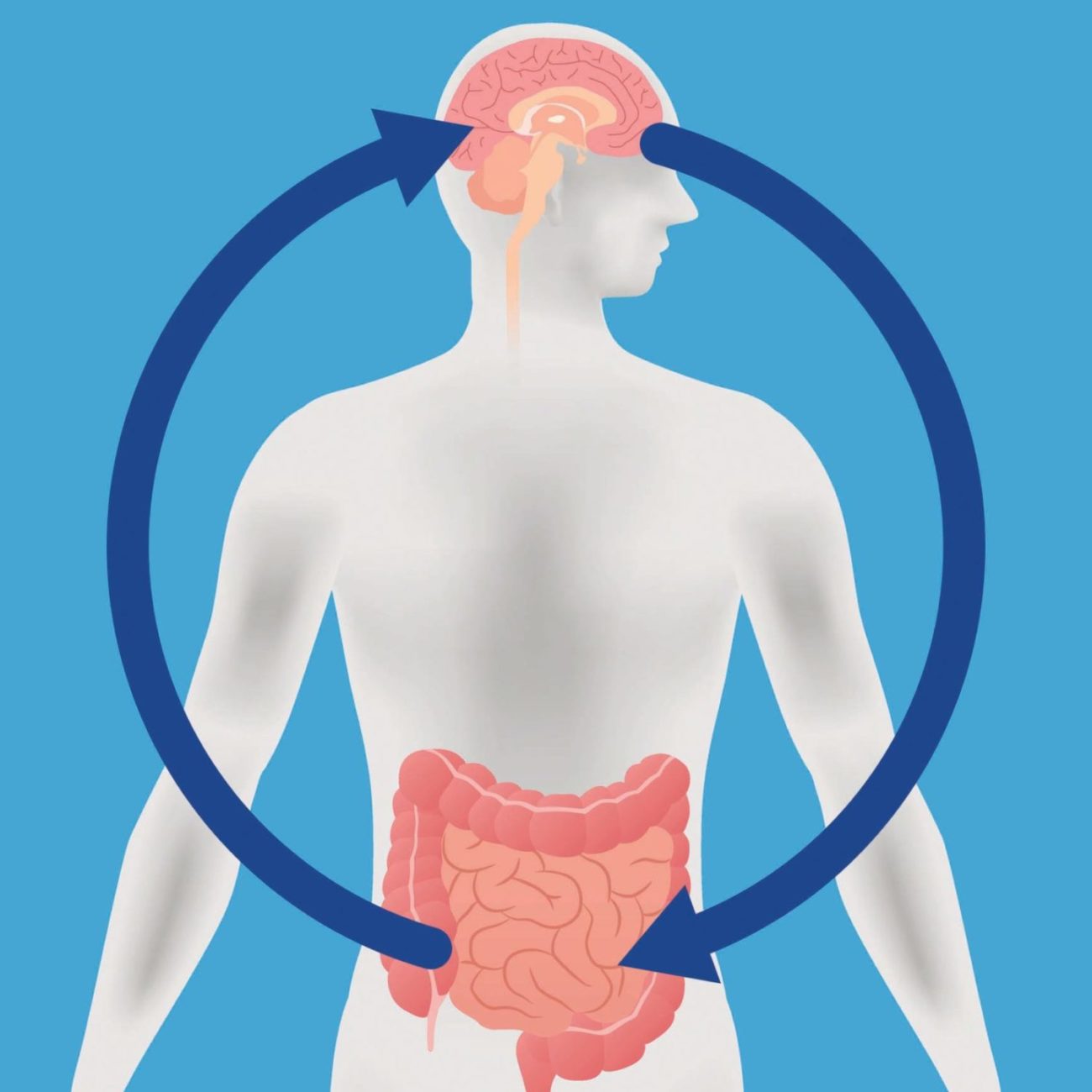
We also know that there is a strong connection between the gut and the central nervous system. In fact, gut bacteria manufactures about 95% of serotonin in the body, which influences mood. (So, the “trust your gut” adage may have some scientific basis.) What’s more, there may actually be a connection between emotional symptoms like depression and anxiety, and gastrointestinal symptoms such as bloating and constipation.
While further research is needed, increasing evidence suggests that short-chain fatty acids produced by gut microbes can bolster gut barrier and immune function, and decrease inflammation.
Okay, so we’ve defined the elusive “gut health,” but what does it have to do with menopause?
What’s the connection between gut health and menopause?
Gut microbiome changes
As sex hormone levels fluctuate during perimenopause, the decrease in estrogen and testosterone can actually change our gut microbiome composition, potentially reducing the microbiota diversity (which is essentially a measure of how many different species of gut microbiota exist in the microbiome and how evenly distributed they are).
Lower diversity is considered a marker of dysbiosis (aka microbial imbalance) in the gut and has been found in people with autoimmune diseases, Irritable Bowel Syndrome, obesity, and cardiometabolic conditions, as well as in elderly people. Research suggests that menopause is associated with lower gut microbiome diversity, which is significant for a couple key reasons…
Reduced estrobolome potential
Not to be confused with estrogen, estrobolome is a subset of microbes in our gut including enzymes that metabolize and regulate the body’s estrogen levels. Specifically, the gut microbiota secretes an enzyme called beta-glucuronidase which reactivates deactivated estrogen in the gut, so that it can be recirculated in the body.
Imbalance in estrobolome and estrogen can impact weight gain, vaginal dryness, hot flashes, brain fog, and a whole other host of menopause symptoms we’re all too familiar with. For postmenopausal women, disturbance in the estrobolome also correlates with heightened risks of obesity, cardiovascular disease, and osteoporosis.
Imbalance in estrobolome and estrogen can impact weight gain, vaginal dryness, hot flashes, brain fog, and a whole other host of menopause symptoms we’re all too familiar with.
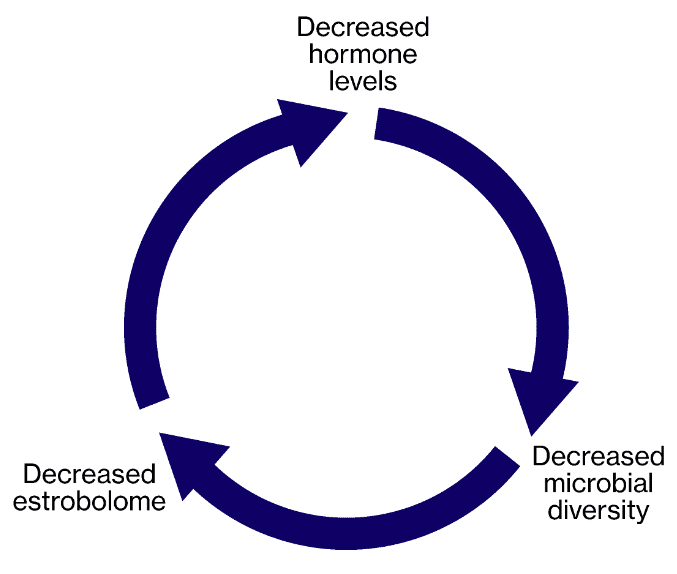
So, what we’re talking about here is essentially a feedback loop: hormone levels decrease and our microbial diversity in turn decreases, which causes reduced estrobolome, which causes further decreases in estrogen levels. And it doesn’t end there – decreasing hormone levels can also change the very composition of our gut barrier…
Gut epithelium changes
The gut epithelium is a barrier surrounding the intestines that is responsible for absorbing nutrients and limits the entry of bad bacteria. As estrogen and progesterone decreases, the barrier can actually become more permeable, allowing microbial translocation to occur (which, in non-science speak, just means that gut bacteria can migrate out of the gut.) That movement of bacteria can activate the immune system and cause inflammation.
What can we do to improve our gut health?
Okay, that was probably a lot to digest. (Yes, we went there.) Now, here are some ways we can bolster our gut health:
1. Up the fiber intake
As you might remember from our fiber article, the nutrient can be classified as either non-fermentable or fermentable, the latter referring to fiber containing prebiotics. Prebiotics are a type of fiber broken down in the large intestine by bacteria. The relationship goes both ways; as the bacteria breaks down the prebiotic fiber, the nutrient actually feeds the microorganisms and encourages the growth of good bacteria. This feeding process in turn maintains estrobolome.
Consuming foods high in fermentable fibers like oats, legumes, and root vegetables is one way we can encourage this feeding process.
2. Prioritize probiotic and fermented foods
In addition to consuming fermentable fiber, eating already fermented foods like kimchi, kefir, miso, and kombucha is a great way to bolster gut health and maintain diversity of good bacteria.
3. Reduce intake of processed food
On top of being generally bad for us given their significant fat and sugar content, processed foods may also impact intestinal function. This is due to the food additives they contain, which can alter the microbiome composition and cause inflammation.
When possible, we recommend avoiding ultra-processed foods. We’re big fans of the Mediterranean diet rich in fresh produce, whole grains, and omega-3 fatty acids (which can also lower risk of heart disease).
What about probiotic supplements?
As with most nutrients, it’s ideal to obtain probiotics directly from food sources. (Supplements can be expensive, hello?!) The American Gastroenterological Association suggests that probiotics are typically only necessary for preterm infants, folks with IBS, and people taking antibiotics, to prevent a gut infection. In these cases, the association recommends the following organisms: S. boulardii (a yeast), Lactobacillus species, and Bifidobacterium species.
It’s important to note that there’s many different bacterial strains, and what’s recommended for someone experiencing gut issues could be different from the appropriate strains for vaginal health. Probiotic supplements also range in volume of live strains included, so make sure to check the level of live bacteria before purchasing.
The bottom line
If it feels like everything is interconnected and, well, complicated — it’s not just you. Digestive health in pre- and postmenopausal women is still a new area of study, as is much of women’s health research, but current insights make clear a few key points.
- Low levels of estrogen observed in menopausal transition are associated with reduced gut microbiome diversity and estrobolome potential, which can inform a range of common menopause symptoms.
- Hormonal changes may increase permeability of the gut barrier, which can trigger an immune system response and inflammation.
Prioritizing fiber is one way we can maintain a healthy gut microbiome, as well as our general well-being
READ MORE: