For a good portion of our life, menopause is one of those “out of sight, out of mind”-type things.
Of course we all know it’ll happen eventually, but it just seems SO far off…until it isn’t. Out of nowhere, it sneaks up on us and then — surprise! — our bodies are changing and our hormone levels are out of control.
Sound familiar? Trust us, you’re not alone — but you are in the right place. Below, we’re breaking down what you need to know about what to expect and how to manage symptoms in order to live well through all of the stages of menopause and beyond.

When, how & why
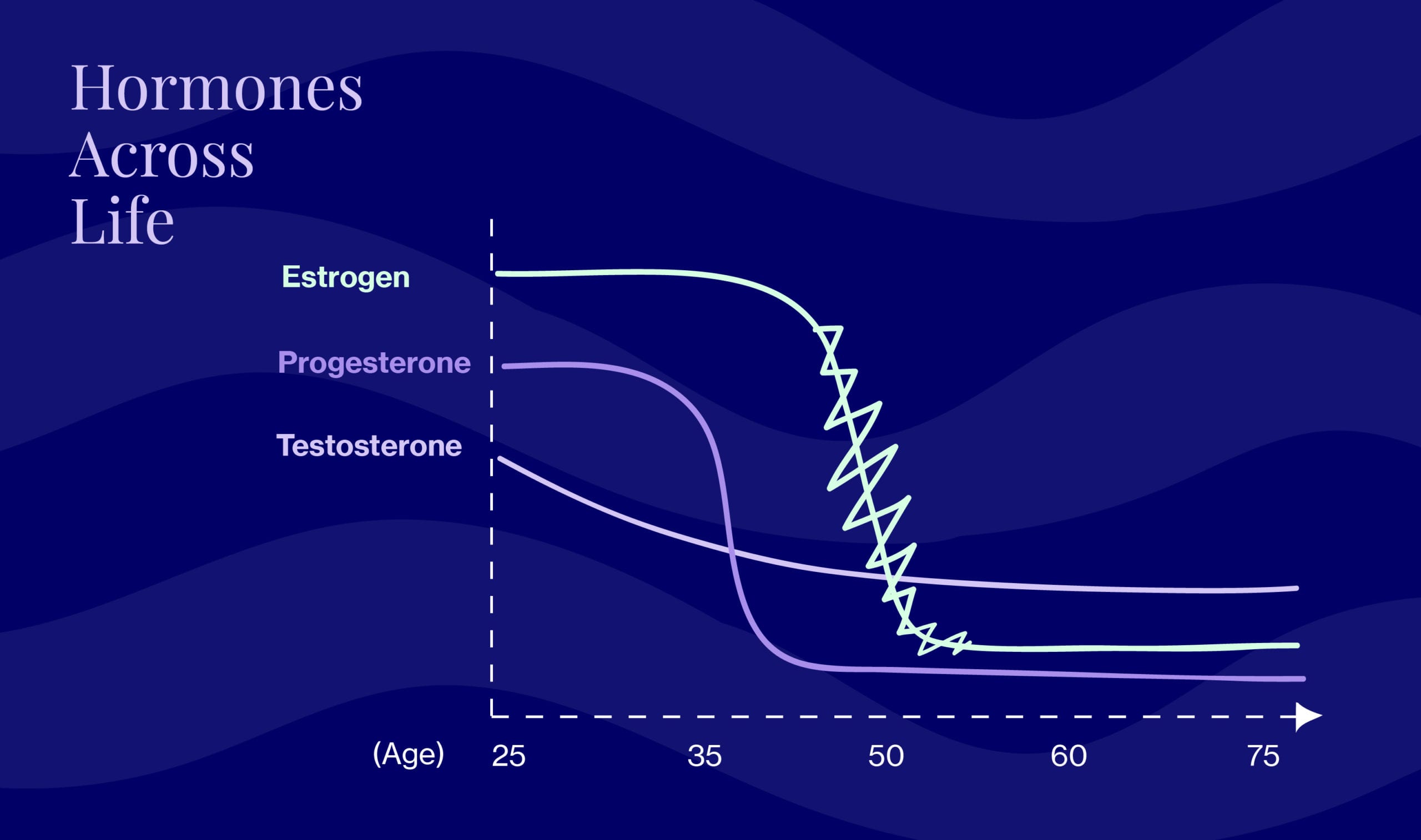
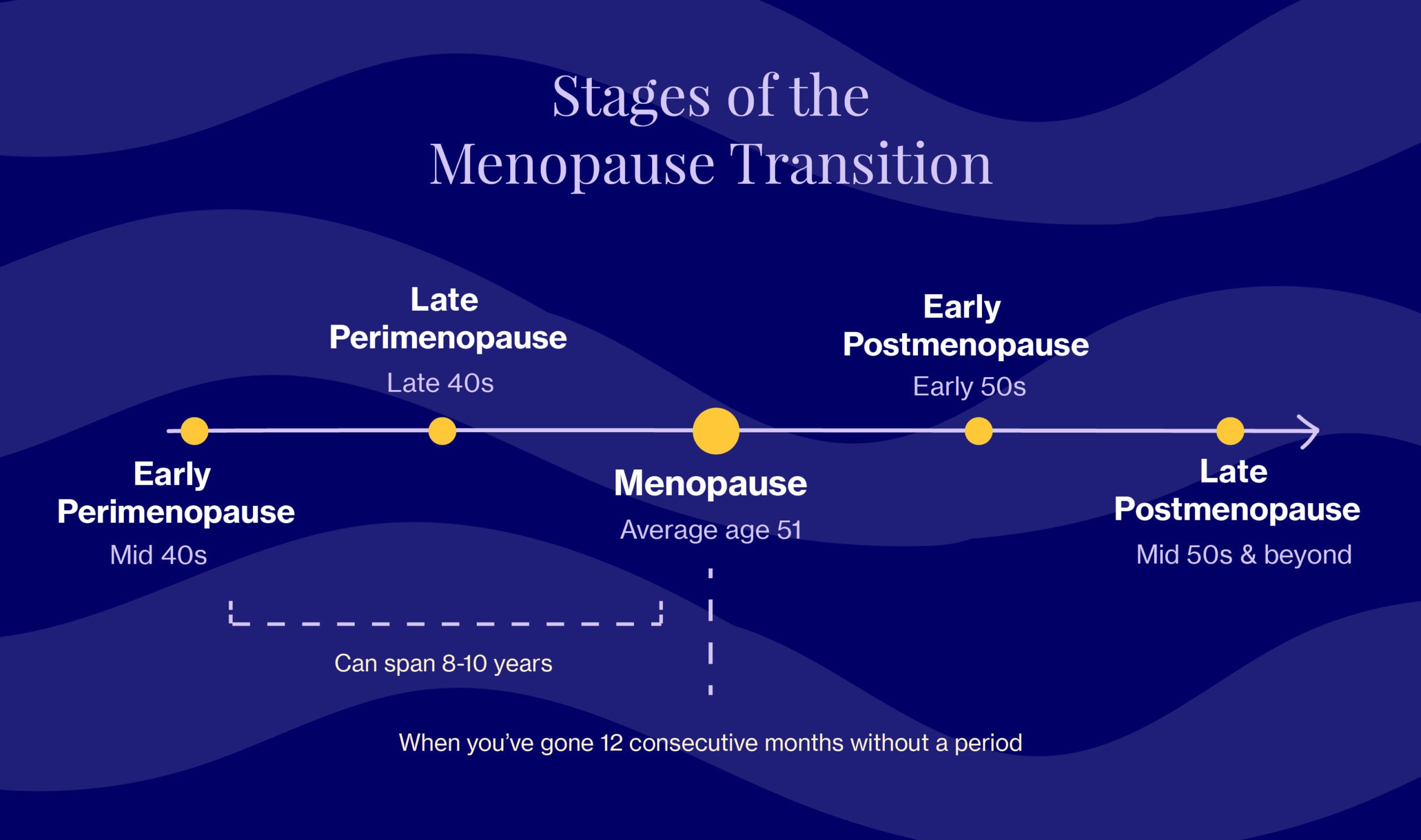
During the menopausal transition, the body’s production of two key female hormones, estrogen and progesterone, begins to progressively decline until you hit menopause which, officially speaking, occurs once you’ve gone 12 consecutive months without a period. Progesterone starts to decline first, and the decline is steep. Estrogen follows the same course but fluctuates a lot as it decreases (picture a roller coaster). Testosterone also declines on a gradual slope.
In Western societies, the average age is ~51, but many women start experiencing symptoms — like irregular periods and hot flashes — upwards of 8-10 years beforehand, during a stage known as perimenopause (aka “around menopause”). Once you’ve hit menopause, ovaries stop releasing eggs and cease production of the hormone, estrogen. You’ll remain here for the rest of your life, an era that’s also described as “postmenopause.”
Many of us assume menopause means we’re destined to feel tired, deflated, and, well, “meh” for years on end, which is simply not the case.
“So many women I’ve talked to see menopause as an ending. But I’ve discovered this is your moment to reinvent yourself after years of focusing on the needs of everyone else. It’s your opportunity to get clear about what matters to you and then to pursue that with all of your energy, time, and talent.” Oprah Winfrey
Perimenopause & menopause symptoms: what to expect
In an ideal world, we’d be able to package the symptoms of perimenopause, menopause, and postmenopause into neat, well-organized boxes that are unpacked one at a time. Unfortunately, menopause isn’t one-size-fits-all, and as Elektra’s founding physician, Dr. Anna Barbieri, MD explains, every woman experiences the transition differently.
“The experience can vary from individual to individual as well as across ethnic and cultural groups and across different countries and regions of the world,” says Dr. Barbieri.
That said, research does point towards certain patterns and trends. For example, we know that the symptoms typically associated with menopause (there are roughly 34) are actually experienced by most women during late perimenopause, peaking during the last two years due to an accelerated drop in estrogen levels. Below are the most common:
- Hot flashes/night sweats
- Irregular periods
- Vaginal dryness & discomfort during sex
- Urinary urgency & incontinence
- Difficulty sleeping
- Emotional changes (e.g., irritability, mood changes, anxiety/depression)
- Dry skin, eyes, or mouth
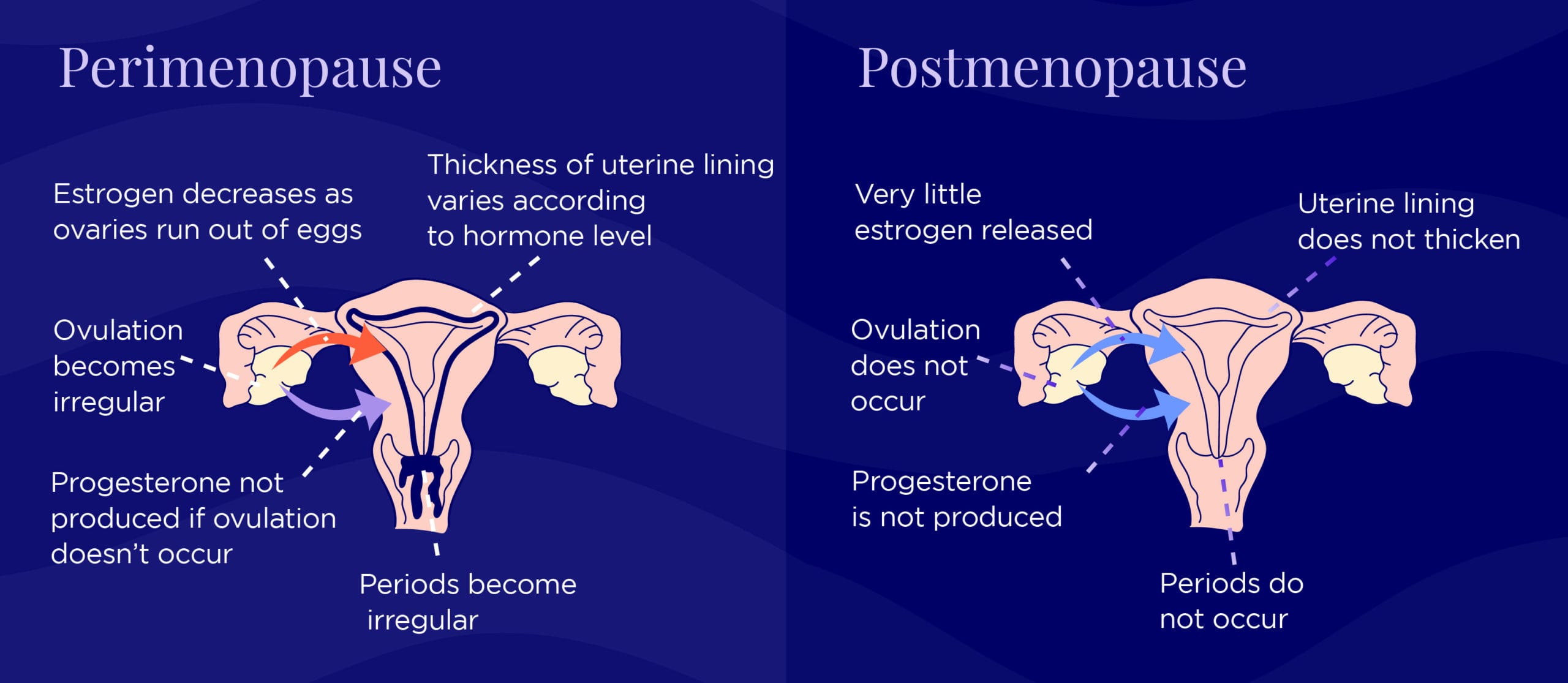
Estrogen, progesterone and your period during the menopause transition.
Interested in learning more about what happens before you officially enter menopause? Look no further than Elektra’s perimenopause primer.
Post-Menopause
After you hit the menopause mark, you officially enter post-menopause. And remember, this is 12 months without a period. Many women will go 8-9-10 months and think they are in the clear, and then BAM, they get a period. And the clock starts over. Frustrating, to say the least.
Once you are post-menopausal, many symptoms tend to subside (hooray!) but some may persist, like vaginal and urinary symptoms (not hooray – but the good news is these can be addressed relatively easily!).
And, unfortunately, there are some longer-term health implications that come with being post-menopausal. We’re subject to increased risk of developing heart disease, diabetes, and osteoporosis.
The menopause transition is therefore THE time to take action every day to help prevent those conditions through self-care, healthy habits, and making sure we’re proactively getting the healthcare we deserve at this point in our lives.
Dr. Anna Barbieri, MD
Pro tip #1
We're big fans of flexing the self-love muscle. Next time you look in the mirror, tell yourself that you love yourself. However silly it may sound at first, trust that the way you speak to yourself impacts your perception of self, especially as your hormones impact your relationship with your body. The more you do it, the easier it'll get, just like any habit.