If, seemingly out of nowhere, your gums hurt when you brush your teeth or your mouth constantly feels dry even though you’re drinking so. much. water. know that it’s not just you.

Oral symptoms during perimenopause are totally a thing, and they can be traced back to those two key hormones we talk about so much: estrogen and progesterone.
Estrogen
What it does:
- Decreases bone resorption (which basically just means “breakdown”)
- Binds to receptors in oral tissues including your salivary glands
What happens during menopause:
Estrogen/oestrogen levels steadily decrease during the menopausal transition, which leads to thinning and weakened oral tissues and gum inflammation.
Progesterone
What it does:
- Supports bone metabolism
- Acts as a bone formation-stimulating hormone
What happens during menopause:
Like estrogen, progesterone levels decline during menopause, which leads to feelings of oral dryness.
Hormone levels themselves may have an impact on mouth bacteria, or something called the “oral microbiome,” although we are just starting to look at and understand this relationship. That may be why our mouths are especially susceptible to hormone fluctuations — even before menopause. In fact, many women experience gum changes during their cycles due to increases in progesterone, which can contribute to bright red swollen gums, swollen salivary glands, the development of canker sores, or bleeding gums…these symptoms usually pop up a day or two before menstruation, only to clear up shortly after the period starts.
Once we hit menopause, hormonal changes may contribute to the following conditions:
Xerostomia (aka dry mouth)
Xerostomia occurs with decreased saliva production, which leads to dry mouth — the most common oral symptom reported in menopausal women. Dry mouth, in turn, can result in periodontal disease since saliva is not readily available to moisten and cleanse the mouth by neutralizing acids produced by plaque.
Burning Mouth Syndrome (BMS)
You’ve just burnt your mouth on a too-hot spoonful of soup or sip of tea — except you haven’t…it just feels that way (think burning, tender, tingling, hot, scalding, numb sensations).
Gingivostomatitis [jin-je-vo-sto-ma-ti-tis]
What a mouthful of a name! (No pun intended.) Gingivostomatitis is a fancy way to talk about inflammation of the gums. It’s characterized by atrophic (terrible clinical term, we know) gums that readily bleed and appear either abnormally pale and dry or shiny and red. Other symptoms include canker sores, bad breath, fever, and swollen lymph nodes. This condition is caused by bacterial and viral infections, and poor oral hygiene.
Any sores lasting longer than 3 days warrant a call to your dentist or doctor.
Periodontitis
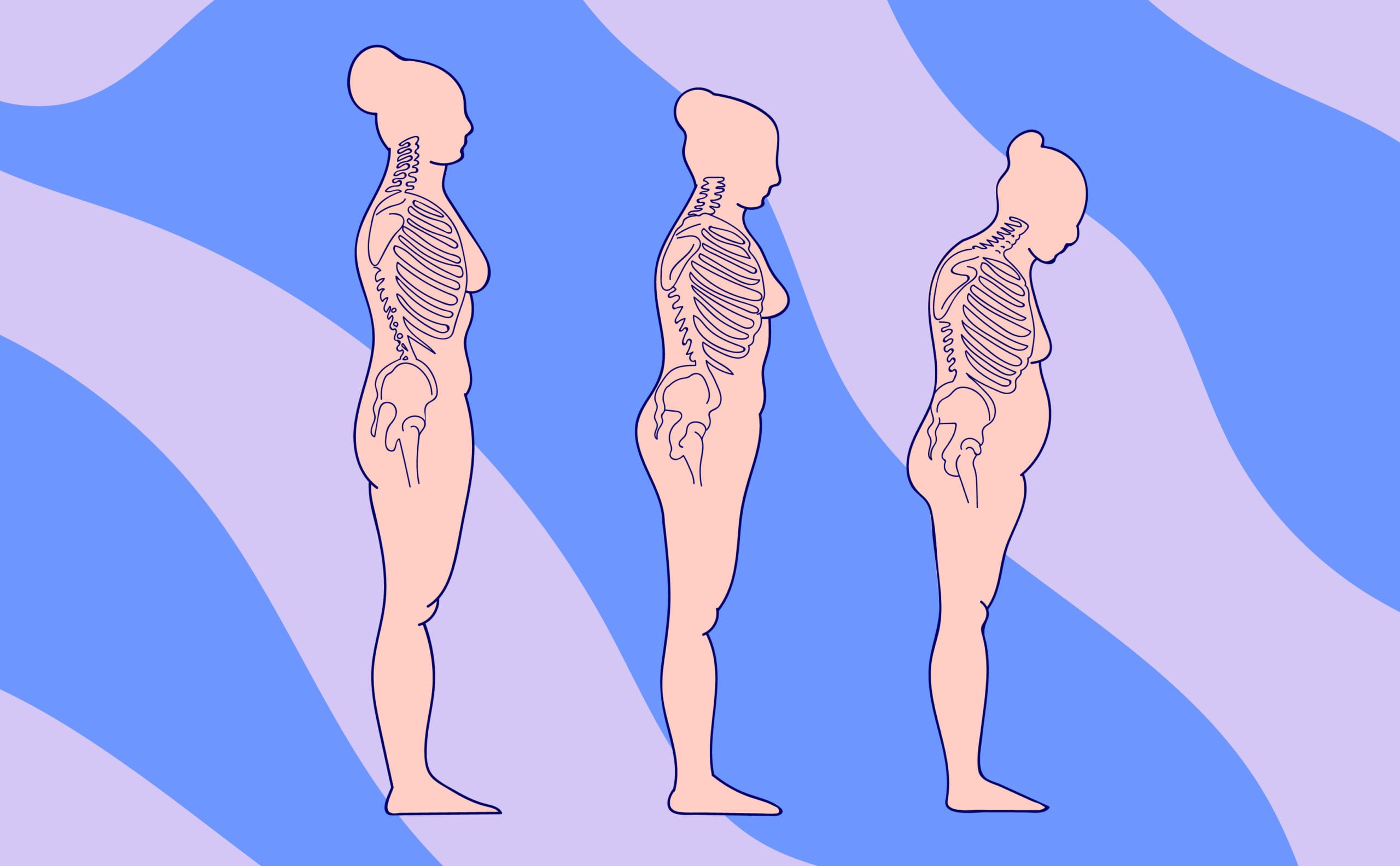
Declining estrogen affects our bone health, putting us at a greater risk for osteoporosis and periodontitis (inflammation of the tissues surrounding the teeth). It can also lead to bone loss in the jaw, which in turn exposes more of a tooth and leads to decay or tooth loss. Not-so-fun fact: osteoporosis makes us three times more likely to experience tooth loss, so it’s definitely important to talk to your healthcare provider (or Elektra!).
Dr. Anna Barbieri, MD
Pro tip #1
Toothpaste with stannous fluoride is particularly good for gum health since it reduces the risk of gingivitis and bleeding (and thus reduces the complications that can come from dry mouth). There is a small risk that this type of toothpaste may stain teeth, but that risk has decreased in recent years with a newly developed formulation. Common household brands like Crest and Colgate make stannous fluoride versions.